- The suprachoroidal space has been explored as a target for IOP reduction for the past 100 years, and the ability to reliably and safely expliot it to lower IOP now seems within reach.
- Recent advances have made it possible to image the suprachoroidal space, and the understanding of its clinical applications is currently being greatly expanded.
- Innovation in eye care over the next few years is almost certainly going to involve utilization of the suprachoroidal space to treat an increasingly wide array of diseases.
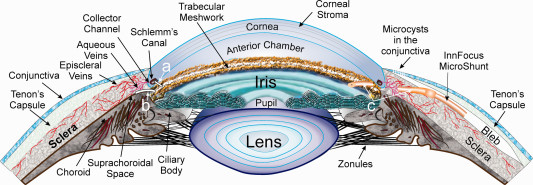
The suprachoroidal space has been explored as a target for IOP reduction for the past 100 years. In 1900, Ernst Fuchs, MD, PhD, described the relationship between ciliary body detachment and low IOP after cataract surgery. Five years later, Leopold Heine, MD, devised the cyclodialysis spatula to reproducibly create a cyclodialysis cleft to lower IOP.
Although early IOP reductions were obtained with this approach, the results were complicated by prolonged hypotony (excessively low IOP), hemorrhage, and profound IOP spikes following spontaneous closure of the cleft. Thus, the procedure was not widely adopted. Although it had become clear that accessing the suprachoroidal space via cyclodialysis clefts was a powerful way to lower IOP a safe and reliable surgical approach remained elusive until recently.
After decades without significant advances in this space, in 1966, James Gills, MD, developed a Teflon implant that was placed ab externo within the cleft to prevent spontaneous closure. However, this device ultimately failed due to difficulty of implantation, profound inflammation, and IOP spikes. Again, interest in this space waned in favor of more traditional subconjunctival approaches to glaucoma surgery.
Fast forward to the 2000's and we find the successful development of a suprachoroidal microshunt, and more than one ab interno supraciliary microstent. Here I would like to highlight a drug-free, non-surgical technique that may be of interest to glaucoma patients.
Drug-Free, Nonsurgical Reduction of Intraocular Pressure for Four Months after Suprachoroidal Injection of Hyaluronic Acid Hydrogel
Abstract
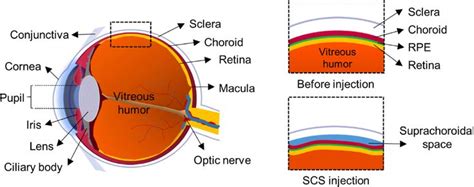
Glaucoma is the leading cause of irreversible blindness. Current treatments use drugs or surgery to reduce intraocular pressure (IOP). In this study, a drug-free, nonsurgical method is developed that lowers IOP for 4 months without requiring daily patient adherence.
The approach involves expanding the suprachoroidal space (SCS) of the eye with an in situ-forming hydrogel injected using a microneedle. This study tests the hypothesis that SCS expansion increases the drainage of aqueous humor from the eye via the unconventional pathway, which thereby lowers IOP.
SCS injection of a commercial hyaluronic acid (HA) hydrogel reduces the IOP of normotensive rabbits for more than 1 month and an optimized HA hydrogel formulation enables IOP reduction for 4 months.
Safety assessment by clinical ophthalmic examinations indicate the treatment is well tolerated. Histopathology shows minor hemorrhage and fibrosis at the site of injection. Further analysis by ultrasound biomicroscopy demonstrates a strong correlation of IOP reduction with SCS expansion.
Outflow facility measurements show no difference in pressure-dependent outflow by the conventional pathway between treated and untreated eyes, supporting the hypothesis.
In conclusion, SCS expansion with an in situ-forming hydrogel can enable extended IOP reduction for treating ocular hypertension and glaucoma without drugs or surgery.
Keywords: glaucoma; hyaluronic acid hydrogels; intraocular pressure; microneedle injections; suprachoroidal space.
- PMID: 33511001
- PMCID: PMC7816721
- DOI: 10.1002/advs.202001908
Free PMC article
.2020 Dec 7;8(2):2001908.
Authors
J Jeremy Chae , Jae Hwan Jung 4 , Wei Zhu 6 , Brandon G Gerberich , Mohammad Reza Bahrani Fard , Hans E Grossniklaus , C Ross Ethier 7 , Mark R Prausnitz 5
Affiliations:
- 1 School of Chemical and Biomolecular Engineering Georgia Institute of Technology Atlanta GA 30332 USA.
- 2 Department of Pharmaceutical Engineering Dankook University Cheonan 16890 South Korea.
- 3 Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University Georgia Institute of Technology Atlanta GA 30332 USA.
- 4 Department of Pharmacology School of Pharmacy Qingdao University Qingdao 266021 China.
- 5 George W. Woodruff School of Mechanical Engineering Georgia Institute of Technology Atlanta GA 30332 USA.
- 6 Department of Ophthalmology Emory University School of Medicine Atlanta GA 30322 USA.
Sources:
The Suprachoroidal Space: The Next Frontier - Glaucoma Today